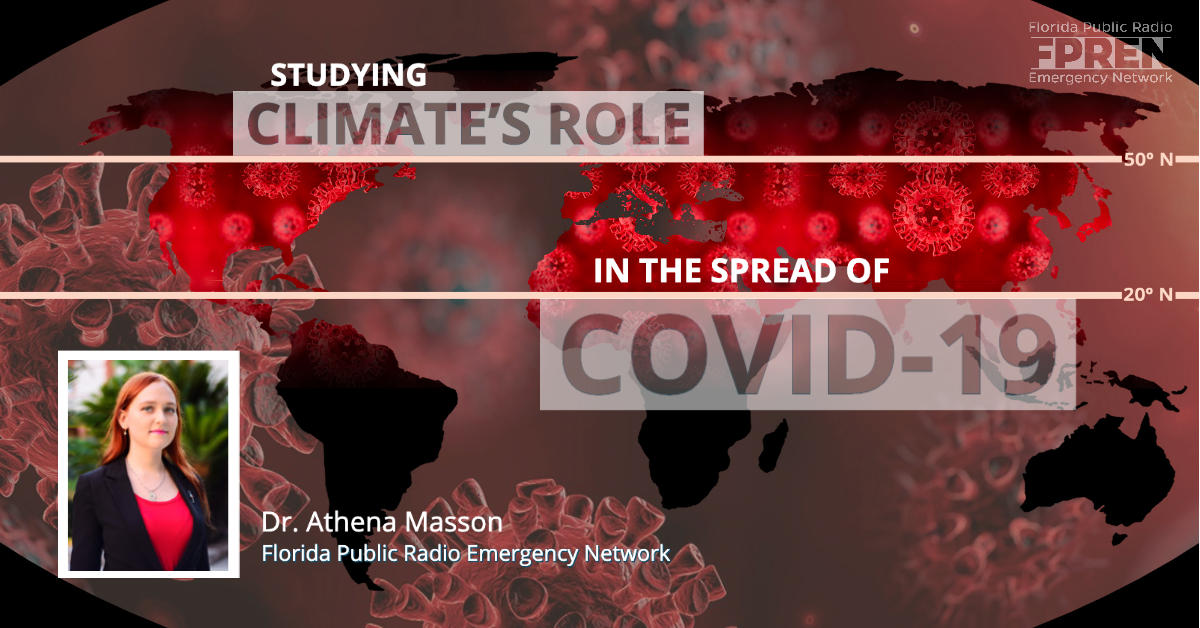
Does Climate Have A Role In The Spread Of COVID-19?
Gainesville, Florida – COVID-19 could be more infectious and deadly than the flu, but only time will tell if the contagion is seasonal.
The rapid spread of the virus has created an urgent need for researchers to find links to its spread. One possible factor is the climate.
Uncertainty on climate’s role
The first case of the virus was detected and reported to the World Health Organization’s China office on Dec. 31, 2019.
A region’s climate could play a role in the spread of COVID-19, but there are less than three months of data for scientists to work with.
Links between temperature, humidity, and the spread of coronavirus are now being monitored closely.
A new study from the University of Maryland hypothesizes that latitudes, along with other temperature and climatological factors, could contribute to the spread of COVID-19.
Some of the worst-hit areas — from China’s Wuhan province, to Iran, Italy, South Korea, and now the United States — are on, more or less, the same latitudinal zone where colder and drier air masses appear to be more conducive to the spread of the virus.
“The major outbreaks we studied as of early March occurred in regions with a very similar latitude and strikingly similar temperature and humidity pattern,” said Dr. Mohammad Sajadi, an associate professor at the University of Maryland’s School of Medicine.
The study examined the spread of COVID-19 across several locations around the world, and it noted that other virus hotspots like China, Iran, Japan, South Korea, Italy, and Washington State, are all located within similar latitudes.
Air temperatures between 41 and 52 degrees Fahrenheit, or 5 and 11 degrees Celsius, appear to be the most conducive to the spread of the virus. Average humidity values between 47 and 79 percent are also noted within the other zones of COVID-19 spread.
“In addition to having similar average temperature, humidity, and latitude profiles also exhibit a commonality in that the timing of the outbreak coincides with a nadir in the yearly temperature cycle, and thus with relatively stable temperatures over a more than a one month period of time,” the authors wrote.
Epidemiologists have hypothesized that a warmer spring and summer may help slow the virus’ spread, mostly due to behaviors in such climates. Dr. Sajadi also agreed that, in general, a warmer spring may temporarily help halt the virus’ spread.
“With a new virus causing a pandemic in a population that has no immunity to it, yes, I would like to see a warmer spring/summer across the U.S.,” says Dr. Sajadi.
Population density likely a bigger factor
A factor that could play a larger role in the spread of the virus may be population density.
The northern hemisphere is the hotspot for COVID-19 at this time. About 88% of the world’s population lives north of the equator due to the increased amount of landmass as compared to the southern hemisphere.
According to Andre Andersen’s World Population Map, most of the population live 27 degrees north of the equator, which puts it right in the heart of the latitudinal zone that COVID-19 is thriving.
Ideal climatological conditions may play a key role in the spread of COVID-19, but it is also important to note that the population density of these latitudinal zones also contributes to the advancement of the virus. The likelihood of the virus spreading increases with population density, thus government officials have taken precautions to minimize the amount of gatherings in the coming weeks and months to help stop the spread of the virus.
Spreading of viruses
Since little is still known on COVID-19, scientists, researchers, government officials, and emergency managers are looking to influenza for similar practices to prevent its spread.
COVID-19 is thought to spread from person to person through respiratory droplets produced by an infected person nearby, according to the Center for Disease Control (CDC). It may be possible that a person can also contract COVID-19 by touching a surface that has the virus on it, then proceeding to touch their mouth, nose and eyes. The CDC says that coughing, sneezing, or even speaking — similar to the flu — can spread the tiny infected droplets to people nearby.
Evidence so far shows the disease kills a larger proportion of people compared to the flu — and it is particularly lethal for people older than 80.
The seasonal flu has a mortality rate of about 0.1% each year, on average. The World Health Organization (WHO) announced that COVID-19 has killed 3.4% of the people who have contracted the virus so far — a mortality rate far higher than the seasonal flu.
In temperate regions, the flu is largely a winter phenomenon, whereas in tropical and subtropical parts of the world the virus tends to occur in the rainy season. Evidence shows that cold and dry air is favorable for the transmission of the flu.
Populations tend to seclude themselves indoors in cold and rainy weather, which will increase the likelihood of contamination.
Spending time outdoors mitigates the threat.
There is the possibility that the summer season will increase melatonin and vitamin D levels, which will help one’s immune system.
COVID-19 may be similar to the flu virus during the summer months and may slow its spread, and possibly its strength, in warmer weather because the fatty coating on the virus begins to degrade.
The WHO, however, says that it is a ‘false hope’ COVID-19 will disappear in the summer like the flu.
“We have to assume that the virus will continue to have the capacity to spread,” says Dr. Mike Ryan, executive director of WHO’s health emergencies program.
“It’s a false hope to say, yes, that it will disappear like the flu. We hope it does. That would be a godsend, but we can’t make the assumption. And there is no evidence.”
COVID-19 in the United States
The number of people who have tested positive for COVID-19 topped 10,000 on Friday in the United States, with 150 deaths from the disease.
The U.S. Centers for Disease Control and Prevention urge gatherings of more than 10 people be canceled for the next eight weeks to slow the spread of the virus. Local governments have encouraged residents to stay home and practice social distancing.
The virus is new territory for medical experts who are struggling to battle the rapid spread.
“We just don’t know enough,” says Dr. Lisa Masson, Medical Director for Cedars-Sinai Enterprise Information Systems Faculty in Los Angeles, California.
The United States has been struggling to test for COVID-19 but the surge of patients is becoming overwhelming.
Dr. Masson describes going into Urgent Care late Monday night and “every. single. patient. Was there with a cough”.
“No, we can’t test you for COVID. The U.S. doesn’t have enough tests. Unless you have a fever…forget about it. If you don’t need to be in an urgent care, stay home,” Dr. Masson explains to patients.
“We can help with nebulizer treatments. We can rule out the flu. We can order a chest x-ray. But we can’t test for COVID (at this time) unless you are Sick. The capital S was intentional.”
Preventative measures
There is currently no specific treatment, cure, or seasonal vaccine for the rampant COVID-19 and although there are many uncertainties health officials say the public can prevent and protect themselves from the virus.
The WHO outlines several standard recommendations to prevent the virus from spreading including regular hand washing, covering mouth and nose when coughing and sneezing, thoroughly cooking meat and eggs.
Regularly and thoroughly wash your hands with soap and water or use an alcohol-based hand rub.
Practice social distancing and maintain at least a 6-foot distance between yourself and others. Avoid close contact with anyone showing symptoms of respiratory illness such as coughing and sneezing.
Avoid touching your eyes, nose and mouth. Surfaces carry can carry viruses and if picked up by hands it can transfer the virus to your eyes, nose or mouth. From there, the virus can enter your body and can make you sick.
If you feel unwell, stay home to prevent spreading the virus to friends, coworkers and family. If you contract a fever, cough and have difficulty breathing, seek medical attention and call in advance.
Follow advice given by your healthcare provider, your national and local public health authority or your employer on how to protect yourself and others from COVID-19.
A full list of recommendations provided by the WHO can be found here.
*Dr. Lisa Masson is related to author Athena Masson and has served as Medical Director for Cedars-Sinai Enterprise Information Systems Faculty in Los Angeles since 2015. Prior to then, Masson served as associate director since 2011. California has the third-highest concentration of cases in the U.S., according to the CDC.
*WKGC is an FPREN station.